- Visibility 1k Views
- Downloads 68 Downloads
- Permissions
- DOI 10.18231/j.jchm.2024.024
-
CrossMark
- Citation
Economics of universal health coverage in India: A comparative analysis
Abstract
The affordability and accessibility of medical services has become a hurdle in a healthy life. This reflects the importance of Universal Health Coverage (UHC). The present paper highlights economic and financial aspects of UHC in India in comparison of countries under study. The study aims to find out the sources of funding UHC in the selected countries and to suggest thorough implementation of UHC in India. The data has been collected through various secondary sources. Countries have been selected based on their higher ranks relative to India in the UHC service coverage index to have a better perspective of UHC implementation. India needs to cover entire population under UHC. Current health expenditure as a percentage of Gross Domestic Product (GDP) and current health expenditure per capita, in India is less than countries under study. This is reflected in high out of pocket expenditure in India. India should focus on more comprehensive UHC. Funds should be efficiently utilized, and more funds need be allocated to the Ayushman Bharat Scheme. Coordination between State and Center Governments is key in extending the area of UHC.
Introduction
Universal health coverage was brought to the forefront of healthcare priorities in 2015 by the United Nations (UN) Member States.[1] As part of the Sustainable Development Goals, Target 3.8 desired nations to “achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.” [1] The World Health Organization (WHO) defines this universal health coverage (UHC) as one that provides access to medical facilities without causing financial difficulties. UHC is an endeavor that many nations have pursued during the last few decades.
The value of UHC in India is demonstrated by the effect of health care expenditure on a large portion of the country. Out-of-pocket expenses have been historically high, significantly affecting many families. [2] Over 17 percent of the population spend more than 10 percent of their income on out-of-pocket health expenses.[3] Low government expenditure and high out-of-pocket expenses contribute to the vicious cycle of poverty.[2] As India is the second largest country in the world with over 1.4 billion people, the health burden is understandably great.[2]
In India, formal discussion of UHC began in 1946, when the Bhore committee recommended the creation of a health system that provides the entire population with accessible, essential care.[4] The government’s commitment to UHC dwindled over time. The central government developed Rashtriya Swasthya Bima Yojana (RSBY) for low-income families in 2008, which covered INR 30,000 of secondary care per family annually.[2] About 41 million families had RSBY coverage in 2016. State Government schemes covered tertiary care, and primary care was completely separate.[2] Having multiple schemes caused detrimental division of risk pools, and out-of-pocket expenditure remained high.[2] In 2010, the Planning Commission of India created the High Level Expert Group to build a plan for affordable, universal health coverage.[5]
India took large strides on the road to universal health coverage in 2017, when Ayushman Bharat was proposed through the National Health Policy 2017 agenda.[2] Ayushman Bharat represents the Indian government’s prime scheme to reach the UN’s Sustainable Development goals. [2] Ayushman Bharat aim to decrease the disease burden and reduce catastrophic expenditure.[2] Pradhan Mantri Jan Arogya Yojna (PM-JAY) covers 40 percent of India’s population, those that economically disadvantaged.[2] As a plan that is fully funded by the Indian government, funding for PM-JAY remains an issue.[2]
Rationale
PM-JAY is the world’s largest free Government health insurance scheme. It is a step towards Universal Health Coverage in India. Apart from rigorous efforts, a huge amount of financial investment is also required to achieve a strong health infrastructure. Being a developing country, financing UHC may be the major challenge for the Government. The present paper highlights economic and financial aspects of UHC in India in comparison to other countries under study.
Materials and Methods
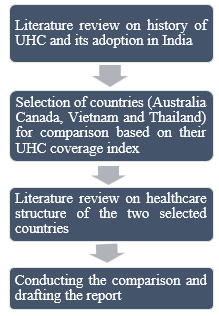
Data has been collected from various sources such as National Health Accounts, PMJAY’s official website. Peer-reviewed articles were examined for information on the development of PM-JAY. In addition, its status on funding and gaps in budget have been analyzed through the Government of India’s Union Budget documents. These documents have been recorded under Expenditure Budgets for the Ministry of Health and Family Welfare. Variance analysis has been performed by subtracting budget from actual expenses for PM-JAY by the central Indian government, if both values were available.
Selection of comparison countries
Four countries that have implemented UHC were selected as comparisons to India. Thailand and Vietnam were chosen in this study because they are also low- and middle- income countries, according to the World Bank.[3] Notably, both Thailand and Vietnam have significantly higher UHC service coverage index scores, a measure that represents access to essential health services, than India. Apart from the low- and middle-income countries, two high income countries (Australia and Canada) were selected for comparison with India to have a holistic viewpoint of implementation for UHC in these selected countries. These countries have also high score on the UHC Coverage Index, created by the World Bank.
Data was reviewed from the literature using literature databases and web searches on six main indicators relating to universal health coverage for India, Thailand, Vietnam, Australia and Canada. These indicators are:
The amount of population covered under UHC.
Total and out-of-pocket health expenditure.
Sources of financing.
Insurance coverage amount.
Service coverage.
Service delivery.
Secondary sources including government websites, peer-reviewed journal articles, Indian news articles, and recognized international sources and The World Bank global data set was used for most available indicators. The utmost care has been taken to fetch the data that is comparable inspite of all the variations in the structure of the healthcare systems of the countries under study to avoid implications of variations.
Brief Overview of the Health Systems
UHC in India
Under National Health Policy 2017, stress was placed on strengthening primary health care along with making quality healthcare services accessible and affordable to all the citizens of the country. In this regard, the Government of India initiated Ayushman Bharat Yojna with two important and interrelated components, Health and Wellness Centers (HWCs) and Pradhan Mantri Jan Arogya Yojana (PM-JAY). Both these components are mainly financed through general tax revenues.[6]
HWCs
HWCs were initiated to provide preventive, promotive and complete primary health. The target is to establish 1,500,000 HWCs under Ayushman Bharat Yojna, as strengthening primary healthcare is a basic approach for UHC. Both variable and fixed costs are needed to set up HWCs. But while allocating budgets, only variable costs were taken into consideration. Thus, less funds were left for infrastructure development. In 2018-19, INR 1200 crore were allotted to HWCs and about 99 percent of this fund was released. During next financial year, this allotment was increased to INR 1600 crore, 33 percent higher than previous year. On the other hand, variable cost was estimated to be INR 1793 crore, which was INR 193 crore higher than the allocation. States are suffering because of this gap of allotted and actual requirements of funds.
PM-JAY
PM-JAY is the world’s largest government-financed health insurance plan that provides cashless secondary- and tertiary-level care. [2] Launched in September 2018, the number of beneficiaries treated grew from five hundred thousand in December 2018 to two million in April 2019 and to three million in June 2019.[2] All ages, pre-existing conditions, and family sizes are covered, based on criteria using the Socio-Economic Caste Census 2011.[2] As of early March 2021, 24,334 hospitals were empaneled, and 139,175,952 e-cards for beneficiaries have been enrolled and processed.6. 16,453,386 hospital admissions have been covered under PM-JAY.
Funding Status for PM-JAY
The original budget for 2019-2020 was 6400 crore INR and was later revised to 3200 crore INR. Despite increasing numbers of beneficiaries, the proposed central government budget for PM-JAY has not been increased from 2020 to 2021. This may lead to negative effects on the government’s ability to carry out its plan for affordable health care. In addition, early state utilization data has shown less uptake and claims from states with proportions of higher poverty and higher disease burden.[7] These issues may be due to problems with implementation across different states, including difficulties with hospital empanelment and beneficiary enrollment.[7] With limitations in budget and difficulties in implementation, PM-JAY has several improvements to make be called as UHC. In India, about 73 percent of entitled households have been covered by either through PM-JAY or state health insurance schemes. Above 80 percent of claims have been centered in 11 states and Union Territories of India.[8]
UHC in Australia
The health system of Australia utilizes a regionally administered Universal Public Health Insurance called the Medicare. Initially introduced in 1973 as a universal healthcare bill in Parliament, the bill for Medicare took ten years to be adopted. In 1975, the bill was partly adopted, making healthcare services free for the retired population who qualified a set of requirements. In 1984, the Medicare system as we see it today was finally established. Medicare is managed at three tiers- at federal level, the state level and by the local government.
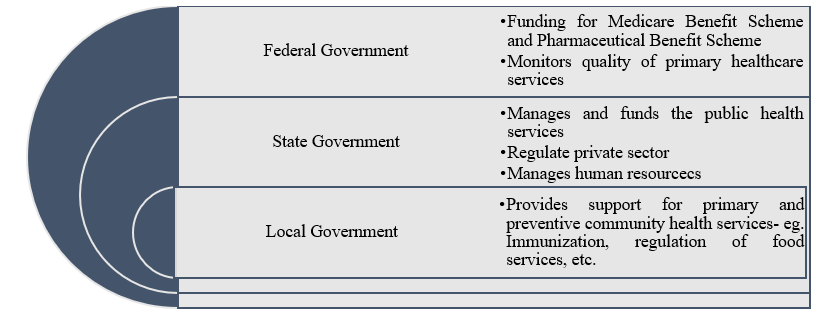
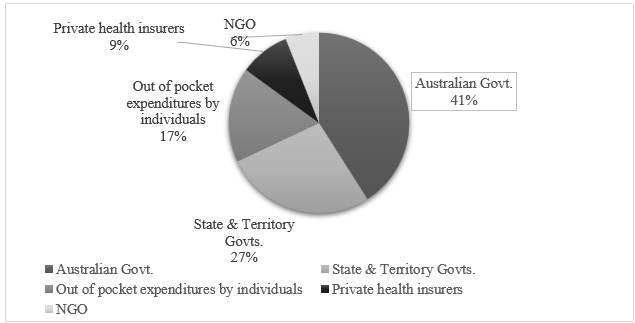
In the year 2021, health expenditure as percentage of GDP was 10 percent. The health system of Australia is complex, and its funding arrangement reflects this. The healthcare system receives funding from all three tiers of the government: non-government organizations, private health insurers and individuals who pay out of pocket for services which are not reimbursed or subsidized. The Medicare is financed mainly through government levy and general tax revenue.
UHC in Canada
The Canadian healthcare system is a decentralized, publicly funded, universal system- termed as Canadian Medicare. Canada witnessed the formation of the Canadian Medicare in 1957 and 1966, when the federal legislations were passed.
The Canadian Medicare is funded and managed by the 13 provinces and territories of the country. Each province/territory (P/T) has its own insurance plan and holds the responsibility of funding, managing, and delivering health services. It is pertinent to note here that benefits and services available under Medicare vary by region in Canada.

In 2022, 12.2 percent of the GDP was directed at health spending. While 71.8 percent of it was accounted for by the public sector, 28.2 percent of the expenditure was accounted for by the private sector.[9] At the level of the P/T governments, government revenue is the main source of funding, most of which comes from taxation. The Canada Health Transfer, the federal program which contributes to the P/T healthcare, provided about 24 percent of the total expenditure.
UHC in Thailand
Health care system in Thailand has a pluralistic public/private mix in both health care providers and financing agencies. However, most of health services were provided by public health care providers. These public health care facilities receive government budget mainly for salary and capital investment and they are allowed to keep their revenue from their services for running their business. Currently, the Ministry of Public Health owns 891 hospitals which cover more than 90 percent of districts and 9,758 health centers, which cover every sub-district. These health services are financed mainly from third party payers. Thailand reaches the universal coverage for health care in 2002.
Thai citizens by law are member of one of social health protection schemes. Civil Servant Medical Benefit Scheme (CSMBS) for central government employees and other small public employee benefit schemes cover 7 percent of population. The Social Security Scheme (SSS) for private employees covers 15 percent of the population, and the rest (76 percent) are in the Universal Coverage Scheme (UCS). The UCS covers everyone who is in informal sector either rich or poor. Thailand is one of the few developing countries in the world that have successfully implemented Universal Health Coverage (UHC).
UHC in Vietnam
Vietnam’s administration is organized across four levels – national, provincial, district, and communes. For health service delivery, there are three major levels of services – primary level with districts and communes, secondary level with provinces, and tertiary level with tertiary hospitals under the central government. The country has covered more than 85 percent of the population under UHC.
Vietnam is one of the countries committed to the UHC 2030 partnership (originally the International Health Partnership, or IHP+), a health partners’ Group that was established in 2004 supports the high-level health policy dialogue among various key stakeholders, including government, development partners, and non-government organizations.
Results
|
Countries |
||||||
|
Parameter |
India |
Thailand |
Vietnam |
Canada |
Australia |
|
|
Population Covered |
40% under PMJAY |
99.33% |
87.70% |
100% |
100% |
|
|
Health Expenditure |
Current Health Expenditure 2019 (% of GDP): 3.01, Current health expenditure per capita, PPP 2019 (current international $): 211, Out-of-pocket expenditure 2019 (% of current health expenditure): 54.78 |
Current Health Expenditure 2019 (% of GDP): 3.79, Current health expenditure per capita, PPP 2019 (current international $): 731.31, Out-of-pocket expenditure 2019 (% of current health expenditure): 8.67 |
Current Health Expenditure 2019 (% of GDP): 5.25, Current health expenditure per capita, PPP 2019 (current international $): 558.87, Out-of-pocket expenditure 2019 (% of current health expenditure): 42.95 |
Current Health Expenditure 2019 (% of GDP): 10.84, Current health expenditure per capita, PPP 2019 (current international $): 5409.7, Out-of-pocket expenditure 2019 (% of current health expenditure): 14.91 |
Current Health Expenditure 2019 (% of GDP): 9.91, Current health expenditure per capita, PPP 2019 (current international $): 5389.8, Out-of-pocket expenditure 2019 (% of current health expenditure): 15.98 |
|
|
|
||||||
|
|
||||||
|
Financing Sources |
PM-JAY: state and federal taxes; state: Central government funding ratio generally range from 40:60 to 10:90, Employee’s State Insurance Scheme: state taxes and employee/employer contributions |
UCS and CSMBS: general taxation; tobacco and alcohol levies, SSS: payroll taxes. |
General revenues; salary contributions |
Provinces/territories pay for approximately 70 percent of expenses. The federal government pays for approximately 24 percent of provincial and territorial health expenditures. |
Universal public health insurance program (Medicare) is financed through general tax revenue and a government levy. |
|
|
|
||||||
|
Coverage Amount |
Varies; PM-JAY: up to Rs. 5 lakh per family per year, Central Government Health Scheme subscription costs: Rs. 250 - Rs. 1000, Employee’s State Insurance Scheme: unlimited coverage |
No copayments, deductibles and extra-billings, No maximum extent of coverage |
Most have a 20% co-payment, but some of the poor have a 0% to 5% copayment |
|
|
|
|
|
||||||
|
|
||||||
|
Services Covered |
once wage limit of Rs. 21,000 is met. Varies since service delivery is governed by the states. PM-JAY: all hospital services, 3 days pre-hospitalization, and 15 days post-hospitalization. Outpatient services and medications are covered under Health and Wellness Centers. Central Government Health Scheme and Employee’s State Insurance Corporation cover a variety of services and medications |
Varies depending on plan but generally comprehensive benefits including outpatient, inpatient, emergency, accident, renal replacement, and rehabilitation services; Depending on the plan, services are provided by contracted public and/or private hospitals |
Care is delivered by two systems: public health center system and acute care system. The public health center system provides preventive and maternal/child services. Inpatient, outpatient, consults, pregnancy visits, and medications are covered. |
General practitioners (GPs), Specialists Hospitals, Prescription drugs, Mental health services, long term care |
Medicare, which includes free hospital care and substantial coverage for physician services, pharmaceuticals, mental health services, long term care etc. |
|
|
|
||||||
|
|
||||||
|
|
||||||
|
|
||||||
|
|
Gaps and recommendations
As demonstrated in Canada, governance at the level of both federal and state allows for addressing issues of equity that may arise due to difference in geographic location, socio-economic variances, and infrastructure status and other similar reasons. In India, usage of the private sector is skewed towards areas that have the least needs in terms of both health and social requirements. Thus, it is necessary for state governments to address the nuances that exist at a regional level to build a more effective healthcare system.
Use of electronic health data in both Australia and Canada assisted in strengthening in their social health insurance programs. The data recorded was utilized in decision-making regarding finances, infrastructure, human resources, equipment and other necessary investments. India can potentially collect and use similar data to guide the development of PMJAY further in the future.
India, Vietnam, and Thailand are all at different stages of the journey to universal health coverage. WHO describes that the health system should have a strong foundation in primary care.[10] The UHC service coverage index was created to measure performance based on this definition and goal, and higher index measures indicate higher achievements in delivering UHC. In 2019, the service coverage index score of Canada and Australia was 89 and 87 respectively followed Thailand was 83 and Vietnam following at 70. However, India fell behind than all the comparators with a service coverage index of 61. This indicates that India has the most opportunity to improve, by learning from the experiences of UHC in other countries.
With UHC, providing access to health services to the entire country is important. Thailand has practically achieved this component fully, whereas Vietnam and India are continuing to work towards this goal. Over 10 percent of Vietnam’s population remains uncovered by the government’s insurance. For India, only 40 percent of the population, or 500 million people, is covered under PM-JAY; total population coverage in the post-PM-JAY implementation period is still to be determined.[2]
The sources of funding for UHC differ country-wise. Whereas most health expenditure in Thailand derives from taxes, a major source of funds in Vietnam and India remain out-of-pocket. India spends the most in out-of-pocket expenditure. Despite these differences, the percentages of GDP spent on health care are almost similar for India and Thailand. When measured in per capita terms, the differences are striking. As of 2019, Australia spends $ 5427.46, Canada spends $ 5048.37, Thailand spends $ 296.17, Vietnam spends $ 180.72, and India spends $ 63.75 per capita on health.[11] India’s spending on health care is still much less than countries under study, even in consideration of its much larger population. The health ministry should ask for more health budget allocation to meet the demand for comprehensive UHC.[12]
Public engagement has been a critical tool utilized across the world to guide the development of health insurance models. It helps record gaps and initiate conversations that users may be facing regarding usage of the system. Adoption of community engagement model in India holds the potential to identify gaps that exist on ground.
Potential explanations for gaps
There are a few potential reasons for India’s gaps in health care financing for UHC. First, India has a much larger population than many countries that have achieved a greater level of universal health coverage. India’s population is 54 times more than Australia, 37 times Canada, 20 times Thailand and 14 times more than Vietnam.
Health care funding has presented a difficult problem due to the large population to be covered.[3] Having less than half of the population insured prior to PM-JAY likely contributed a significant portion to India’s low UHC service coverage index. In addition, more than half of the beneficiaries eligible for PM-JAY have yet to receive e-cards signaling their enrollment.[6] Implementing requirements for health insurance may be a step forward to expand coverage. Secondly, government revenue plays a major role in each health care financing system. For India, there is a smaller tax base which gives less room for health care expenditure.[13], [14] The GDP per capita (Current US$) in 2021 is 2257 for India, 7066 for Thailand, 3756 for Vietnam, 60443 for Australia and 51988 Canada.[4] This indicates that there is less funding available to spend on an individual’s health in India in comparison to other countries under study. Thailand’s transition to fully tax-based insurance schemes and subsequent reduction in out-of-pocket payments should be useful in this endeavor.[9] Lastly, India has had a lack of centralization that has been detrimental to its prior insurance schemes. In Vietnam, for example, there is a single risk pool for its beneficiaries of social health insurance and unified administrative mechanisms.[7] Greater unification of state plans, regulated copayment policies, and regulation of providers in India would be beneficial.
Limitations
Due to variations in the structure of the healthcare systems of each country, direct comparisons were difficult to make. Differences in number and type of insurance schemes as well as the amount of publicly available data limits extensive comparisons.
Since Ayushman Bharat – PM-JAY was more recently enacted compared to UHC in the other selected countries, latest and more detailed data points regarding its impact was unavailable.
Conclusion
Providing affordable healthcare through UHC is one important segment of sustainable Development Goals. Most countries in the world are committed to providing quality health care to their citizens without any financial hardship through UHC. India initiated UHC with Ayushman Bharat Scheme in 2018. All other countries under study have covered almost all the population under UHC, but India has covered 40 percent of population till date. It will be termed as real UHC only when all the citizens are getting affordable healthcare in the country under the scheme. Higher integration of state plans and regulation of providers in India would be favorable for the effective implementation of Ayushman Bharat. The health packages need to be updated on a regular basis based on the needs of the people. Apart from the high allocation of funds as percentage of GDP, there should be efficient utilization of resources with the target of covering the entire population under Ayushman Bharat. The successful implementation of UHC will help India in reducing high out of pocket expenditure on health in the country.
Future research direction
The wide scope of UHC economics creates further directions of research such as cost effectiveness of the various models of UHC and the health packages provided under it, impact of UHC on equitable access to healthcare services, affordability and sustainability, and the contribution of UHC in the overall growth of the country and wellbeing of the people. Researchers may contribute to the knowledge in any of the dimensions of UHC economics.
Source of Funding
None.
Conflict of Interest
None.
References
- . The Australian Health System,” Australian Government Department of Health (Australian Government Department of Health). . 2020. [Google Scholar]
- . About Pradhan Mantri Jan Arogya Yojana (PM-JAY). Ayushman Bharat. 2021. [Google Scholar]
- . World Development Indicators. The World Bank.. . 2023. [Google Scholar]
- . . . . [Google Scholar]
- . Official website of Pradhan Mantri Jan Arogya Yojana (PM-JAY). Government of India. . 2023. [Google Scholar]
- Zodpey S, HF. Universal Health Coverage in India: Progress achieved & the way forward. Indian J Med Res. 2018;147(4):327-9. [Google Scholar]
- Tangcharoensathien V, Aree J, Witthayapipopsakul W, Viriyathorn S, Kulthanmanusorn A, Patcharanarumol W. Political economy of Thailand's tax-financed universal coverage scheme. Bull World Health Org. 2020;98(2):140-5. [Google Scholar]
- . Universal Health Coverage. National Health Portal. . 2023. [Google Scholar]
- . Universal health coverage. . 2023. [Google Scholar]
- . Universal Health Coverage. World Health Organization.. . . [Google Scholar]
- Martin D, Miller A, Vallée A, Caron N, Vissandjée B, Marchildon G. Canada's universal Health-care system: Achieving its potential. Lancet. 2018;391(18):30181-9. [Google Scholar]
- Le Q, Blizzard L, Si L, Giang L, Neil A. The evolution of social health insurance in Vietnam and its role towards achieving universal health coverage. Health Policy Open. 2020;1. [Google Scholar]
- Shroff Z, Marten R, Ghaffar A. On the path to Universal Health Coverage: Aligning Ongoing Health Systems Reforms in India. BMJ Global Health. 2020;5(9). [Google Scholar]
- Summan A, Stacey N, Hofman K, Laxminarayan R, Jamison D, HG, et al. Disease Control Priorities: Improving Health and Reducing Poverty. . The International Bank for Reconstruction and Development. . [Google Scholar]
How to Cite This Article
Vancouver
Bakshi O, Bui Y, Kumar S. Economics of universal health coverage in India: A comparative analysis [Internet]. J Community Health Manag. 2024 [cited 2025 Sep 28];11(3):143-149. Available from: https://doi.org/10.18231/j.jchm.2024.024
APA
Bakshi, O., Bui, Y., Kumar, S. (2024). Economics of universal health coverage in India: A comparative analysis. J Community Health Manag, 11(3), 143-149. https://doi.org/10.18231/j.jchm.2024.024
MLA
Bakshi, Ojaswini, Bui, Yvonne, Kumar, Sumesh. "Economics of universal health coverage in India: A comparative analysis." J Community Health Manag, vol. 11, no. 3, 2024, pp. 143-149. https://doi.org/10.18231/j.jchm.2024.024
Chicago
Bakshi, O., Bui, Y., Kumar, S.. "Economics of universal health coverage in India: A comparative analysis." J Community Health Manag 11, no. 3 (2024): 143-149. https://doi.org/10.18231/j.jchm.2024.024
