Introduction
Prior to the mid-1950s, early umbilical cord clamping was defined as clamping within one minute of birth, while late clamping was defined as clamping more than five minutes after birth.1 However, due to observations of blood volume changes after birth and the lack of recommendations regarding optimal timing, early cord clamping became common practice, usually occurring within 15-20 seconds of birth. More recent studies have evaluated the effects of immediate versus delayed umbilical cord clamping, including randomized controlled trials of term and preterm infants, as well as physiologic studies of blood volume, oxygenation, and arterial pressure. 2
In the 21st century, as preventive healthy interventions become more challenging, evidence-based practices for new born care must be adopted more efficiently in rural care facilities. Awareness of delayed umbilical cord clamping and early skin-to-skin contact should be taught to expectant mothers in all perinatal-neonatal care units nationwide. There is a long-standing debate about when the umbilical cord should be clamped in term infants.3 Recent studies have shown that Delayed Cord Clamping (DCC) is beneficial, and many professional organizations and experts recommend a delay of at least 30 seconds before clamping.4
Delayed Cord Clamping is a birth practice where the umbilical cord is clamped after the pulsation have stopped. Early skin to skin contact involves placing the dried naked baby prone on the mother's bare chest immediately after birth, often covered with a warm cloth.5, 6 A comparative study between ECC and DCC was carried out on a select group of primigravida without any high-risk factor and delivering at term.
Delayed cord clamping (DCC) and early skin-to-skin contact (ESSC) are methods that promote attachment between new-borns and their mothers. These techniques are essential for exclusive breastfeeding and ensuring that the new born stays warm and comfortable and reducing the risk of postpartum haemorrhage and the need for blood transfusion to the mother. 7, 8, 9, 10
DCC with Immediate skin-to-skin contact between the mother and newborn after birth is important for bonding, placental release, breastfeeding, and lowering the risk of postpartum haemorrhage. 11 This article will summarize the effects of early versus delayed cord clamping on the health of the mother. 12
Need of the study
Clamping the umbilical cord too early may lead to issues for the mother. 13 Some evidence suggests that early clamping raises the chances of postpartum haemorrhage and retained placenta because it fills the placenta with the baby's blood.14, 15 This makes it more difficult for the uterus to contract and expel the placenta.
Early cord clamping and separation of mother and newborns after birth can be harmful to both. Delayed cord clamping and early skin-to-skin contact are important interventions that can improve breastfeeding success, keep the newborn comfortable and warm, and offer various advantages for both infants and mothers. 16, 17
Benefits of the study
Studies indicate that close contact between a mother and her newborn can positively influence the baby's connection to the world. The skin, our body's largest organ, receives various sensory signals. Delayed cord clamping (DCC) and early skin-to-skin contact (ESSC) involve placing the baby on the mother's chest, leading to changes in both their bodies. 18
Research indicates that mothers who have immediate skin-to-skin contact with their babies after delayed cord clamping (DCC) produce more milk compared to those with early cord clamping. Also, mothers without skin-to-skin contact are more likely to face disruptions in breastfeeding. 19, 20, 21, 22
Delayed cord clamping (DCC) and early skin-to-skin contact (ESSC) have been proven to boost the mother's rate and duration of exclusive breastfeeding. This approach enhances psychological and emotional well-being, strengthens the bond between mother and infant, and reduces maternal stress. Involving parents actively in caring for their baby increases their confidence and satisfaction. In general, delayed cord clamping (DCC) and early skin-to-skin contact (ESSC) contribute to physiological stability and support the health and well-being of both the mother and the infant.23, 24, 25
Materials and Methods
Ethical consideration: Ethical clearance for conducting the study has been given by the Institute Ethics committee, Banaras Hindu University and obtained to collect the necessary data, based on the present study findings. Written informed parental consent was obtained after assignment to the labour room from the women who were eligible and willing to participate.
Research design and setting: This a randomized control study design. There were two groups- one having intervention in the form of DCC and ESSC while other group having ECC. This needs to be clarified from the authors. We conducted structured interviews to gather data about participants' demographic information and obstetric history. We included women in the study who had a normal and uncomplicated vaginal birth at full term and agreed to participate. We compared factors such as estimated maternal blood loss, temperatures, haemoglobin levels, and breastfeeding behaviour. The study was conducted in labour room and postnatal units of Sir Sunder Lal Hospital, Banaras Hindu University, Varanasi, Utter Pradesh.
Sample size and data collection: We included a total of 300 mothers and their newborns in the study after receiving the mothers' consent. The participants were divided into two groups of 150 each. Group A experienced delayed cord clamping and early skin-to-skin contact, while Group B underwent early cord clamping. Group A comprised women aged between 20 and 40 years, with pregnancies lasting 37 to 42 weeks, along with their newborns. Group B was a matched set of women and their newborns who experienced uncomplicated normal births at the same institution between November 2019 and June 2020.
The criteria for selection of participants were as follows:
The study included women in labour and their newborns who met specific criteria:
Result
This study contained 300 mothers without any complications. They were divided into two groups: one with delayed cord clamping as Group A and the other with early cord clamping as Group B. We observed for any post-birth issues, such as bleeding, and monitored the mothers' blood levels. We are comparing factors such as estimated maternal blood loss, temperatures, haemoglobin levels, and breastfeeding behaviour.
There was a significant difference observed in maternal blood loss during delivery, postnatal maternal haemoglobin levels, or the occurrence of abnormal maternal outcomes (such as postpartum haemorrhage) between both the early and delayed cord clamping groups. Additionally, the amount of blood lost by the mothers during childbirth show a significant difference.
Table 1
Descriptive statistics for temperature of mother
|
Temperature (°F) in both groups |
No. |
Mean ±SD |
Std Error Mean |
|
Group A |
150 |
97.72 ± 0.61 |
0.050 |
|
Group B |
150 |
97.86± 0.61 |
0.049 |
In Table 1, Group A, the mean temperature of mothers was 97.72°F, with a standard deviation of 0.61°F and a standard error mean of 0.0496°F. Similarly, in Group B, the mean temperature was slightly higher at 97.860°F, accompanied by a standard deviation of 0.6055°F and a standard error mean of 0.0494°F.
Table 2
Test statistics for temperatures of mothers
|
Pair |
z-value |
P-value |
|
Group A vs Group B |
-2.177 |
0.031 |
The test statistics comparing the temperatures of mothers between Group A and Group B reveal a corresponding p-value of 0.031. This indicates that there is a statistically significant difference between the two groups in terms of maternal temperatures. We have evidence to reject the null hypothesis, supporting the assertion that there is a significant disparity in maternal temperatures between the two groups [Table 2].
Table 3
Sample statistics for pulse of mother
|
Pulse |
No. |
Mean ± SD |
Std Error Mean |
|
Group A |
150 |
85.93 ± 3.40 |
0.278 |
|
Group B |
150 |
85.64 ± 3.30 |
0.270 |
In Table 3, summarizes maternal pulse statistics for two groups, A and B. Group A has a mean pulse of 85.93 ± 3.40, Std. Error Mean =0.278), while Group B shows a slightly lower mean of 85.64 ± 3.30, Std. Error Mean =0.270).
In Table 4, suggests that there is no significant difference between the compared group A and group B. In statistical hypothesis testing, a p-value greater than 0.05 indicates that there is insufficient evidence to reject the null hypothesis. Therefore, with a p-value of >0.05, we cannot confidently predict or assert a significant difference in mothers' pulse rates between delayed and early cord clamping.
Table 5
Sample statistics for respiration
|
Pulse |
No. |
Mean ± SD |
Std Error Mean |
|
Group A |
150 |
19.99 ± 2.21 |
0.180 |
|
Group B |
150 |
20.17 ± 2.32 |
0.189 |
In Table 5, presents sample statistics for respiration rates in two groups, Group A and Group B. Group A has a mean respiration rate of 19.99 breaths per minute with a standard error of 2.21. In contrast, Group B exhibits a slightly higher mean respiration rate of 20.17 breaths per minute, also with a standard error of 2.32.
The p-value for the respiration test comparing Group A and Group B is > 0.05, it indicates that there is no significant difference between the two variables. Therefore, with a p-value of 0.513012, we would not be able to predict or conclude that there is a significant difference between Group A and Group B in terms of respiration [Table 6].
Table 7
Sample statistics for Haemoglobin (HB)
|
Pulse |
No. |
Mean ± SD |
Std Error Mean |
|
Group A |
150 |
10.27 ± 1.23 |
0.100 |
|
Group B |
150 |
11.15 ± 0. 87 |
0.071 |
Outlines sample statistics for Haemoglobin (HB) levels in two groups, Group A and Group B. Group A has a mean HB level of 10.27. In contrast, Group B displays mean HB level of 11.15 (Table 7).
The p-value for the test of means comparing haemoglobin in Group A and Group B which represents an extremely small p-value <0.05. This small p-value suggests strong evidence to reject the null hypothesis, indicating a significant difference between the means of haemoglobin levels in Group A and Group B [Table 8].
Table 9
PPH descriptive statistics
|
Group |
Mild |
Moderate |
Severe |
Total |
|
Group A |
135 |
09 |
06 |
150 |
|
Group B |
64 |
58 |
28 |
150 |
|
Total |
199 |
67 |
34 |
300 |
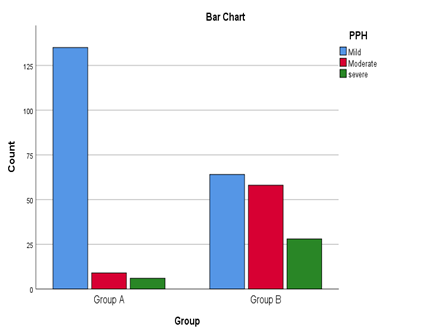
In [Table 9] and [Figure 1] Group A displays a lower risk profile for Postpartum Haemorrhage (PPH), with the majority experiencing mild cases (135), followed by moderate (9) and severe (6). In contrast, Group B exhibits a more diverse distribution, with 64 cases of mild, 58 of moderate, and 28 of severe PPH. Notably, Group A stands out for its higher concentration in the mild category, suggesting a comparatively lower risk of severe PPH compared to Group B.
Table 10
Chi-Square Tests for PPH
|
Test statistics |
Value |
df |
p-value |
|
Pearson Chi-Square |
75.403 |
2 |
0.000 |
Observe that in [Table 10] the p-value is less than the conventional significance level of 0.05, we reject the null hypothesis, indicating a significant association between Group (A and B) and PPH category (Mild, Moderate, and Severe). This suggests that the distribution of PPH categories differs significantly between Group A and Group B.
Table 11
Descriptive statistics for breast feeding
|
Pairs |
At low risk for breast feeding |
At risk for breast feeding problems |
At risk for breast feeding failure |
|
Group A |
135 |
12 |
3 |
|
Group B |
90 |
47 |
13 |
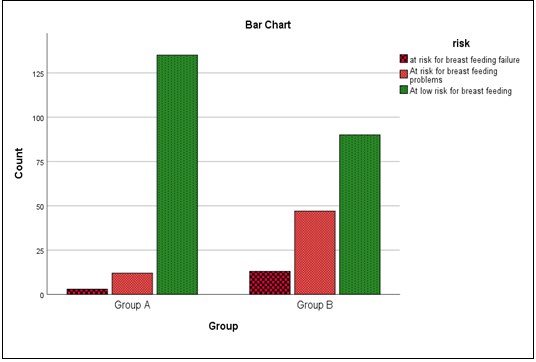
In examining the deceptive statistics [Table 11] and Graph [Figure 2] for Group A and Group B, we observe distinct patterns in the distribution of risk levels related to breastfeeding outcomes. In Group A, a notable proportion, 135 individuals, fall under the category of " At low risk for breast feeding," indicating a predominantly lower risk in this group. In contrast, Group B exhibits a more varied distribution, with 90 individuals classified as " At low risk for breast feeding," but a higher number, 47 individuals, categorized as " At risk for breast feeding problems." Additionally, 13 individuals in Group B are identified as " at risk for breast feeding failure." These findings suggest that Group A leans toward a lower risk profile, particularly in terms of risk for breast feeding concerns, compared to Group B.
Table 12
Chi-Square Tests for Breast feeding risk
|
Test statistics |
Value |
df |
p-value |
|
Pearson Chi-Square |
36.013 |
2 |
0.000 |
Since the p-value is less than the conventional significance level of 0.05, we reject the null hypothesis. The rejection of the null hypothesis suggests that there is a significant association between the risk level (low risk, at risk, at risk for breastfeeding failure) and the groups (Group A, Group B). In simpler terms, there is evidence to suggest that the distribution of risk levels is not the same across Group A and Group B [Table 12].
Discussion
Regarding maternal outcomes, there is evidence to suggest that the timing of cord clamping has an impact on the incidence of postpartum haemorrhage or any other adverse outcome. In a recent study, researchers discovered that waiting for 1-5 minutes before clamping the umbilical cord after a newborn's birth had positive effects on the health of both the mother and the baby. Mothers who underwent delayed cord clamping and early skin-to-skin contact with their newborns experienced significant improvements in temperature, haemoglobin levels, breastfeeding and a reduced risk of postpartum haemorrhage.
Conclusion
Mothers who received Delayed Cord Clamping (DCC) and Early Skin-to-Skin Contact demonstrated modest but statistically significant improvements in vital physiological parameters over two days. This suggests that the strategy of DCC and early skin-to-skin contact can provide enhanced care to mothers without the need for special equipment.
These findings support the broader adoption of the Delayed Cord Clamping (DCC) and Early Skin-to-Skin Contact (ESSC) strategy. It is considered the standard of care for mothers without risk factors. However, the implementation of DCC and ESSC at birth has not been optimal so far. The study indicates that practicing delayed cord clamping and skin-to-skin care leads to improved haemoglobin levels, reduced risk of postpartum haemorrhage, and a higher proportion of exclusive breastfeeding at the time of hospital discharge.