Introduction
Urinary Tract Infection (UTIs) remains one of the most common bacterial infections occurring in medical practice despite the widespread availability of antibiotics. 1
It is also the most common nosocomial infection in many hospitals and accounts for approximately 35% of all hospital-acquired infections.Escherichia coli is the predominant uropathogen. Other organisms known to cause urinary infections are Klebsiella species, Proteus species, Staphylococcus species, Enterobacter species.,Pseudomonas aeruginosa, Acinetobacter species., Enterococcus species., Candida albicans. The emergence of antibiotic resistance in the management of UTIs is a serious public health issue. The easy availability of antibiotics in the community without prescription make the drugs subject to abuse.2 Presence of risk factors like elderly age, diabetes ,immunosuppression, and other comorbidities also makes the treatment challenging. 3 Distribution of uropathogens and their antimicrobial sensitivity patterns may differ regionally so it becomes necessary to study and compile their data in a particular setting. The physician must have sufficient information about the pathogen and its susceptibility patterns so that appropriate empiric antibiotic therapy can be initiated. 4, 5
The aim of this study was to analyze the data to determine the prevalence of the bacterial isolates and change in their sensitivity pattern in urinary tract infections over last 5 years from January 2018 to December 2022 in this setting.
Materials and Methods
A record based observational cross sectional conducted in Microbiology department at Nanavati Max Super Speciality Hospital, Mumbai after getting clearance from Institutional ethical committee with letter no BNH/0246/2023. The urine samples from patients with suspected urinary tract infections (UTI) received in the laboratory from January 2018 to December 2022 were processed by standard laboratory methods. The sample plates which yielded a colony count of bacteriuria. The identification and antibiotic susceptibility test (AST) for the bacterial isolates was done by theVITEK2 automated system (bioMerieux, Durham, North Carolina).
The antimicrobial agents were tested and interpreted as per Clinical and Laboratory Standards Institutes (CLSI) guidelines (M100-edition 33rd 6.Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853
Results
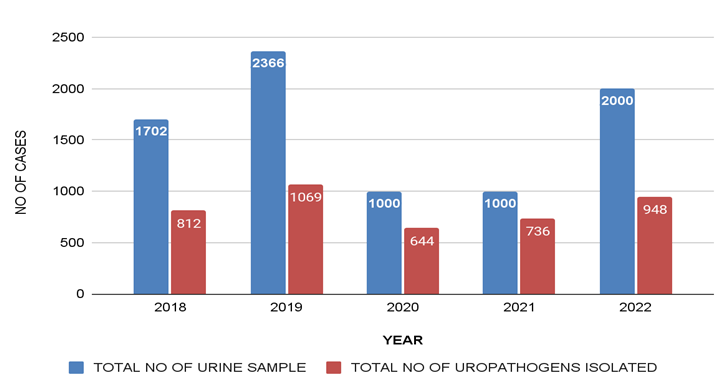
Out of 8068 urine samples, uropathogens were isolated in 4209 (52.16%) samples [Figure 1].
Of the total 4209 urine samples that showed the significant bacterial growth ,1347 (32%) samples were from male patients and 2862 (68%) from female patients. In female patients, high prevalence was seen among 31 to 45 year age group and in male patients high prevalence was seen among >45 year age group.[Table 1]
Table 1
Age and gender wise distribution wise of pathogens
|
Age |
Gender(n=4209) |
|||
|
|
Male |
Female |
||
|
|
No |
% |
No |
% |
|
<18 years |
84 |
2% |
126 |
3% |
|
18-30 years |
84 |
2% |
379 |
9% |
|
31-45 years |
126 |
3% |
1347 |
32% |
|
>45 years |
1053 |
25% |
1010 |
24% |
|
Total |
1347 |
32% |
2862 |
68% |
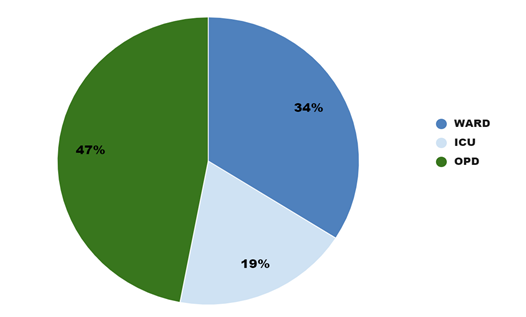
Majority of culture positive isolates were obtained from IPD patients which included 1432(34%) from wards and 815 (19%) from Intensive care units (ICUs). This was followed closely by 1962(47%) isolates from OPD samples [Figure 2].
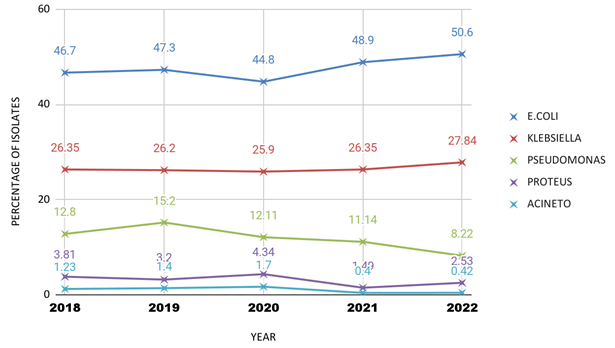
E. coli was the most commonly isolated uropathogen, with a prevalence of 380(46.7%) in 2018 and 480 (50.6%) in 2022 of the total samples. This was followed by Klebsiella species, with prevalence of 214(26.35 %) in 2018 and 264(27.84%) in 2022. Other gram negative organisms isolated were Pseudomonas species, Proteus species and Acinetobacter species [Figure 3].
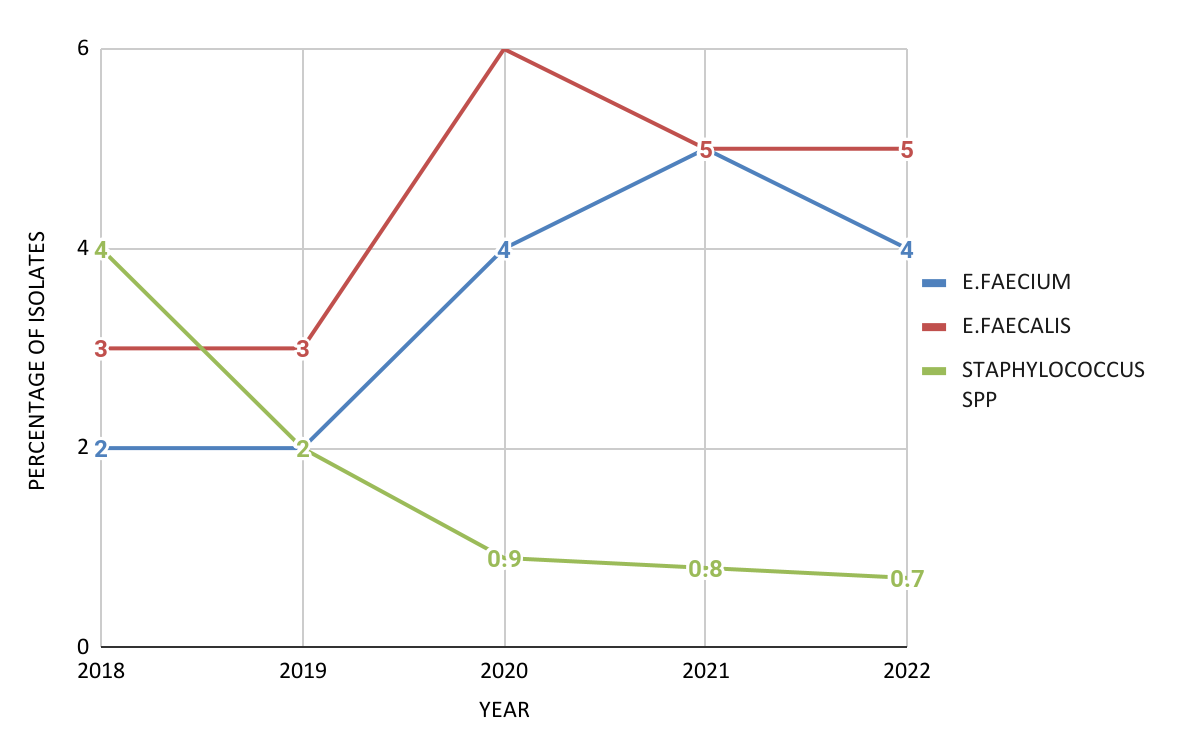
Gram positive cocci isolated were Enterococcus faecalis, Enterococcus faecium and Staphylococcus spp. The prevalence of Enterococcus species increased from 41(5%) in 2018 to 87(9%) in 2022 whereas Staphylococcus species decreased from 32(4%) in 2018 to 7(0.7%) in 2022 [Figure 4].
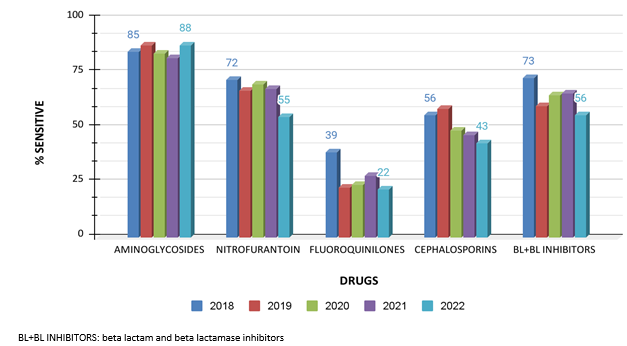
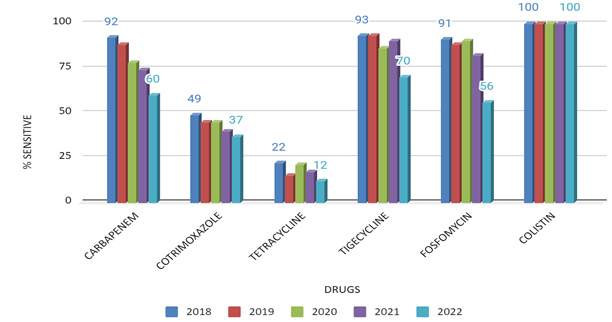
Figure 5, Figure 6 are representative of the overall antibiotic sensitivity pattern of Enterobacteriaceae isolated. In 2022, the Enterobacteriaceae showed high sensitivity to Amikacin(88%) Tigecycline(70%) and Meropenem(60%).This pattern stayed consistent since 2018.
Amongst the cephalosporins, cefuroxime and ceftriaxone showed low sensitivity over the years whereas cefepime showed sensitivity ranging from 54% in 2018 to 60% in 2022. Cefoperazone and sulbactam had sensitivity of 74% in 2018 which reduced to 56% in 2022.
However, sensitivity to antibiotics commonly used in UTI like Fosfomycin, has reduced from 93% in 2018 to 56% in 2022 and sensitivity to Nitrofurantoin has reduced from 72 % to 55%.
In 2022, the Enterobacteriaceae showed considerable resistance to Fluoroquinolones (22%), Co- trimoxazole(37%) and Tetracyclines(12%). Resistance to colistin was not reported during this period.
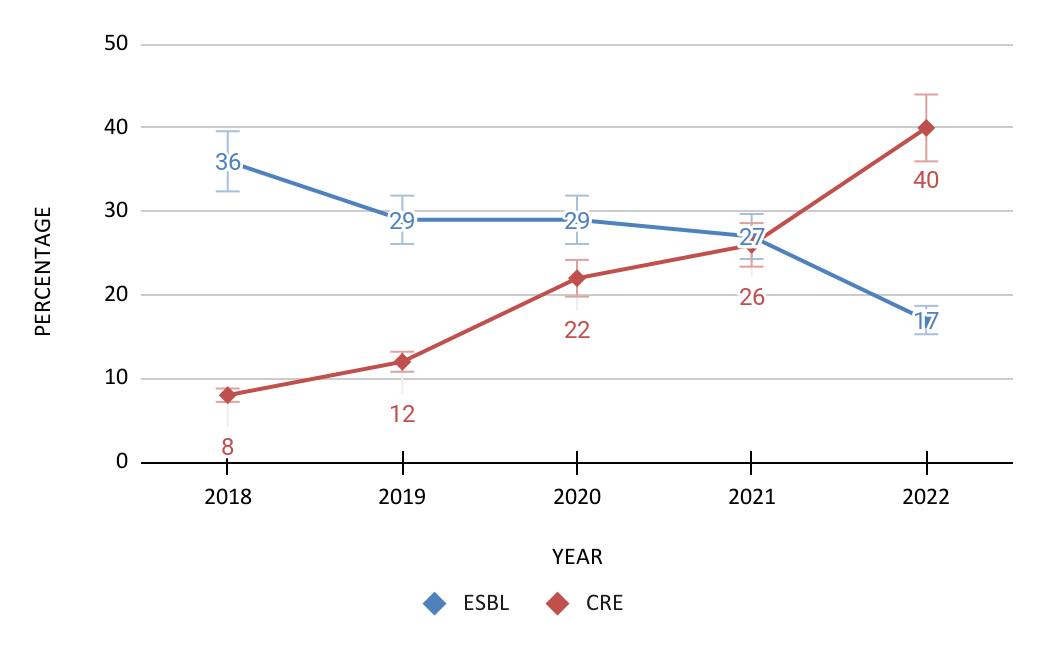
In 2018, from total Enterobacteriaceae (594) isolated, 213(36%) were ESBL producers and 48 (8%) were Carbapenemase producers. In 2022, from total Enterobacteriaceae (745) isolated, prevalence of ESBL producers reduced to 127(17%) and Carbapenemase producers increased to 298(40%)[Figure 7].
Figure 7
Change in pattern of ESBL & CR Enterobacteriaceae isolated in urine over the period. (2018-2022)
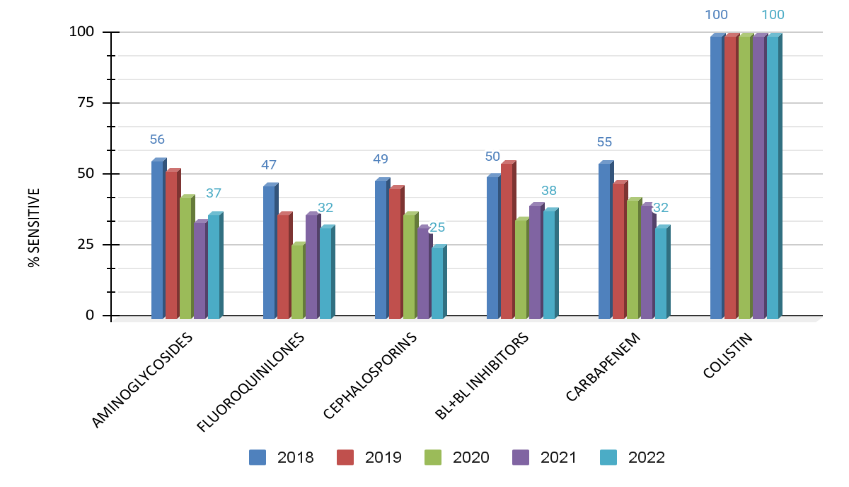
Similar to findings in 2018, the Lactose Non fermenting(LNF) gram negative bacilli like Acinetobacter species, Pseudomonas species and Proteus species had low sensitivity to Fluoroquinolones(32%), Cephalosporins(25%) and Piperacillin Tazobactam(38%) in 2022 also.
There is also an increase in resistance to Carbapenems and Aminoglycosides group of antibiotics. By 2022 only 32 % of total LNF were sensitive to Carbapenems and 37% sensitive to Aminoglyscosides. Resistance to Colistin has not been reported so far in them [Figure 8].
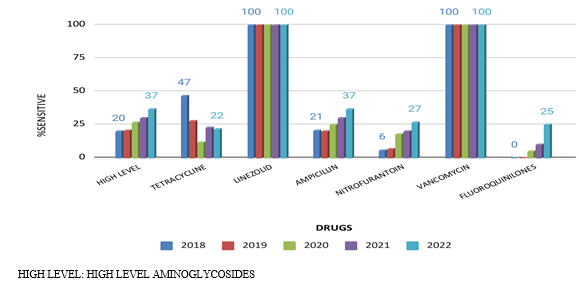
Amongst the gram positive cocci, Enterococci species and Staphylococcus species showed 100% sensitivity to Linezolid and Vancomycin throughout the study. Enterococcus species showed low sensitivity to Nitrofurantoin (6%), High level Aminoglycosides (20%), Fluoroquinolones (0%) and Ampicillin (21%) in 2018. But in 2022, 27 % were sensitive to Nitrofurantoin, 37% to High level Aminoglycosides, 25% to Fluoroquinolones and 37 % to Ampicillin [Figure 9]. Only tetracycline group showed a decrease in sensitivity from 47% to 22% over the five years.
Discussion
Even with the adequate precautions, preventive measures and the advances in therapy, UTIs still remain the commonest infections, both in the hospitalized patients and in community settings. History of antibiotic use prior to referral, such hospitals often face the problem of partially treated or maltreated patients. In the study over 5 years, 4209 uropathogens were isolated from a total of 8068 urine samples, with an overall culture positivity of 52%. This is much higher when compared to other studies, where a positivity of only 15-20% has been observed.7, 8
Of the total 4209 uropathogens isolated ,1347 (32%) samples were from male patients and 2862 (68%) from female patients. Khan MI reported similar finding in their study concluding that females are at higher risk of UTI than males. 9 In concurrence to a study conducted in same city, female patients show higher prevalence among 31 to 45 year age group and in male patients high prevalence was seen among >45 year age group.8
In this study, 2247 (53%) isolates were from IPD patients and 1959(47%) were from OPD patients. In contrast, Gajdács, M et al. report 54% of isolates from OPD and 46% from IPD patients in a study that spanned over ten years. 10 Amongst OPD patients, voided (midstream) urine samples were common, whereas in IPD patients, catheter collected urine samples were common followed by voided(midstream) specimen.
E.coli is the most commonly isolated organism throughout the study. Out of 948 isolates in 2022, 481(50.6%) were E.coli followed by 264(27.84%) Klebsiella species. However in other studies, though E.coli is the most commonly isolated, gram positive organisms like Enterococcus species and Staphylococcus species are the second most commonly isolated uropathogens 7, 10, 11, 12 Over the study period, prevalence of Staphylococcus species reduced whereas that of E. faecalis and E. faecium increased which is in comprehension to studies based in North and South India which also report Enterococcus as the most common Gram-positive bacteria followed by Staphylococcus. 13, 11 Infection due to Enterococcal strains presents a significant medical problem, since they are known to be multi drug resistant,with Vancomycin resistance increasing in prevalence among E. faecium isolates.14
A study in 2018 observes high susceptibility of Enterobacteriaceae to Tetracycline, Cotrimoxazole and Nitrofurantoin.8 In the same year, Jagadeeswaran G et al., Gagan Chooramani et al. and Syed Mustaq et al. recommend Nitrofurantoin as first line agent for UTI in OPD patients in view of high sensitivity of commonly isolated uropathogen towards it.13, 11, 15 In contrast, significant resistance has been observed to these drugs all through the study. Also, since sensitivity of Enterobacteriacea to Nitrofurantoin has reduced from 72 % in 2018 to 55% in 2022, it cannot be advised as first line agent for treatment of UTI in this setting.
Susceptibility of Enterobacteriaceae to Amikacin, Carbapenems and Tigecycline is in concurrence with other studies.8 Resistance to Fluoroquinolones has been observed in all studies 11, 8 An increase in resistance to Cephalosporins and prevalence of ESBLs is same as observed in other studies11, 15 There is a significant reduction in sensitivity to Carbapenems over the period. The irrational and the prophylactic use of these antibiotics in the past few years with inadequate dosage and duration could be responsible for this. The easy availability and the over the counter sale of the antimicrobials without a proper prescription is also responsible for development of resistance to first line agents.
Amongst the Lactose Non fermenters, a rise in resistance to Carbapenems and Aminoglycosides was observed over the years unlike findings of similar studies by Md Aqib Ali Faraz et al. and Syed Mustaq Ahmed et al. which do not report resistance to these group of antibiotics.16, 15 Also low sensitivity has been observed for Fluoroquinolones and Cephalosporins in the present study. In contrast Shivani gupta et al. observed highest sensitivity to Fluoroquinolones.
Resistance to Colistin was not observed in contrast to a study from Southern India where colistin resistance among gram negative bacilli has been reported. 11
Enterococcus species and Staphylococcus species showed 100% sensitivity to Linezolid and Vancomycin. However, Inês Linhares et al and Gajdács M et al reported resistance to these antibiotics amongst gram positive cocci. 7, 10 Though sensitivity to Nitrofurantoin was observed to be much lower than other studies, the sensitivity to High level Aminoglycosides, Fluoroquinolones and Ampicillin is similar to other studies. A rise in susceptibility to these group of antibiotics has been observed over the course of the study 10, 11, 16 Since these antibiotics are not commonly used for UTI now, this has led to decrease in resistance against them.
A continuous surveillance is essential to understand if these antibiotics can be prescribed for empirical treatment in the future. Repeated use or prolonged exposure to the antibiotics could be the reason for development of resistance against the above mentioned antimicrobial agents. Unwarranted use of antibiotics damages periurethral flora, resulting in colonization of uropathogens and subsequent infection of the urinary tract. It also enables bacteria to exchange their genetic material like resistant genes via horizontal gene transfer resulting in spread of resistance to a particular antibiotic. Before prescribing an empirical antibiotic treatment therapy, an in depth understanding of the prevalent organisms and their susceptibility patterns is essential to avoid irrational drug usage and to ensure optimal prophylactic therapy.
Limitation
Since this is a retrospective study based on analysis of previous urine culture and sensitivity reports, we could not trace the patient's clinical settings. Thus features such as catheterization, comorbid conditions like diabetes were not taken into consideration.
Conclusion
The antibiotic sensitivity of uropathogens changes over time and place and this emphasizes a need for regular surveillance and monitoring of their pattern.
Educating patients in the community setting regarding compliance to prescribed drug regimen and avoiding over the counter antibiotics is necessary to avoid misuse of antibiotics.
Since these organisms exhibit resistance to many first-line drugs used for UTI infection, appropriate therapy based on individual bacterial culture and sensitivity reports is essential to curb the rise in resistant strains.