Introduction
No country in the world, not even the one with the most robust of health care delivery systems, has been able to insulate itself from the impact of Covid 19. Most of the nations are still having to make difficult decisions in prioritizing the health needs of their people according to the available resources and providing the basic healthcare to their populations. In the early phases of the pandemic, most of the healthcare systems had been able to maintain routine service delivery in addition to managing a relatively limited COVID-19 caseload. As the number of cases of Covid increased, so did the demands on the health care systems. Furthermore, the already scarce health care work force became increasingly exposed to COVID-19 infection. Strategic adaptations were then made by the governments world-over to ensure that limited public and private sector resources provide the maximum benefit to the populations.1
As a result of this, the response to Covid 19 has, at times and to varying extent, negatively affected the provision of routine and essential healthcare services. The second round of a World Health Organization “pulse survey“ reveals that over one year into the COVID-19 pandemic, substantial disruptions persist, with about 90% of countries still reporting one or more disruptions to essential health services, marking no substantial global change since the first survey conducted in the summer of 2020.2 The apartheid between the developing and the developed nations has become more apparent in the response the countries were able to mount to combat the pandemic. The dignity of human life still continues to be somewhat compromised- more so in the resource scarce settings.3 The study of history of pandemics reveals that the direct and indirect mortality due to a new outbreak increases as the health systems are overwhelmed by demands on them4 A similar scenario has been seen as direct mortality due to Covid 19 infections and indirect mortality due non-addressed, preventable and treatable conditions have risen while the healthcare systems continue to grapple with health situations due to Covid 19 and access to routine health care services remains compromised.
Although attempts were made and continue to be made to ensure continuity of essential health services during the pandemic, these could, at best, be partially successful due to various reasons like redeployment of health care personnel to provide COVID-19 relief and restrictions on health facilities and services imposed in line with the guidelines.
This paper is an attempt to assess the state of essential health services in district Amritsar as the 2nd wave of Covid 19 currently grips the nation.
Material and Methods
This descriptive cross- sectional survey was conducted online through google forms after taking clearance from the Institutional Review Board and the august offices of the Civil Surgeon of district Amritsar. The questionnaire was adapted from the World Health Organization-Pulse Survey on Continuity of Essential Health Services during Covid 19 pandemic. The Continuum of essential health care services was graded on a four point Likert scale with grade 1 meaning complete disruption in health services (>50% of usual service capacity), grade 2 meaning partial disruption (5-50% of usual service capacity), grade 3 being no disruption in health services (of usual capacity) and grade 4 being do not know stating uncertainty in commenting on state of continuity of essential health services.
The questionnaire consisted of both close ended and open-ended questions. The respondents were health care personnel working in designated Covid Vaccination Centers in the public and private health care institutions. At the time of conduction of the survey, there were 16 Primary Health Centers or higher hierarchy level operational Covid Vaccination Centers in public health sector and 76 Ayushman Bharat empaneled private health care institutions in district Amritsar. Informed consent was taken and confidentiality of the information was assured. Responses were received from 08 out of 16 public and 47 out of 76 private health care institutions. Descriptive and inferential statistics were applied to quantitative data using SPSS v.22 and the answers to open ended questions were analyzed using Taguette software .
.
Table 1
Distribution of essential health services disruption in public and private health sector.
Figure 1
Distribution of levels of disruption in imaging and radio diagnosis services among public and private health sector
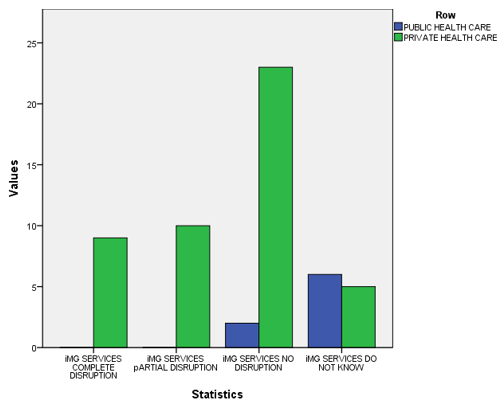
Figure 2
Distribution of levels of disruption in antenatal care services among public and private health sector
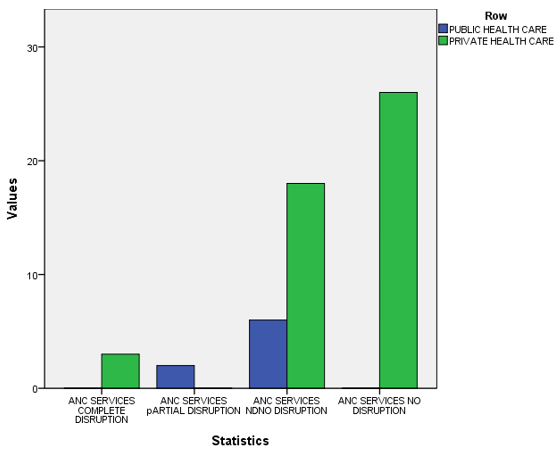
Table 2
Causes for disruptionin essential health services (multiple responses)
Observations
Antenatal care is among the most fundamental of health care services. The World Health Organization mandates a minimum of 8 Antenatal contacts with a skilled health care professional for the expectant mother.5 During the second wave of Covid 19, there appeared a highly significant difference in accessing antenatal health care services in the public and private health care institutions (Mann Whitney U statistic= 78.00, p=.004). This finding was in consonance with the results from a study conducted in Ethopia which found that almost all components of the essential mother and child care suffered in the pandemic.6
A significant toll on maternal and newborn health has taken place during the pandemic. One of the reasons was relative or absolute absence of access to institutional delivery service. Due to the fact that routine health care is disrupted as a result of unavoidable shocks, health system collapse, or intentional choices made in responding to the pandemic, the increase in child and maternal deaths has occured.7 A significant difference in institutional births was observed between the public and the private sector (Mann Whitney U statistic= 112.00, p=.046). The routine immunization services, non-communicable disease screening and treatment services, routine laboratory services, blood bank services, emergency services and dental services were not seen to be affected significantly differently in the public and private health sector institutes. A highly significant difference was observed between the public and the private health care sector in imaging and radio diagnosing services (Mann Whitney U statistic= 48.00, p=.000), A similar finding was made in a study in a health institute in China which found that during a 10-week time period corresponding to the COVID-19 pandemic surge, 65.4% of scheduled block-weeks were disrupted. Low clinical volume was the predominant driver of schedule disruption.8 Financial difficulties faced during outbreak/lockdown appeared to be the most commonly cited reason for disruption in access to essential health services. This was followed by insufficient health care man power to provide the health care services. This was also concluded by a study conducted in Copenhagen.9 Closure of the outpatient department services as per the state directive and decrease in patient volume were the third most common cited reason for disruption of health care services.
There appeared a significant difference (Mann Whitney U= 94.00, p <.05) between the levels of satisfaction about the work performance between the public and private sector. The open ended question seeking answers to what more could have been done to minimize the disruption in continuity of essential health services were analyzed using Taguette, an open source free software for qualitative analysis. The thematic analysis of the collected data yielded the following themes in order of frequency.
Creating a robust public health care infrastructure including e-health in the district
Recruitment of health care manpower according to set norms
Recognition and financial incentives for health care workers doing extra work
Provision of health insurance to the private health care professionals working in Covid 19
Establishing better partnerships and transparency between public and private health sector
Regular training of health care workers
Conclusion
Capacity building and a responsive health care system, maintaining population trust in the capacity of the health system to safely meet essential needs and to control infection risk in health facilities are the keys to ensuring appropriate care-seeking behavior and adherence to public health advice vital to defeating the Covid 19 pandemic.
