Introduction
Diabetes, a lifestyle disorder due to disarrayed glucose metabolism, i.e. defects in insulin secretion, insulin action, or both. It is quickly catching on in India, with more than 77 million diabetic individuals currently diagnosed with the disease.3
Hypoglycemia, espcecially iatrogenic, is a fearful occurrence in individuals with diabetes, and it impairs it’s management. Reduced neurogenic symptoms, a key feature of hypoglycemia unawareness, are largely the result of reduced sympathetic neural responses to falling glucose levels.4
In view of no available statistics in the population in this area, it would be not only interesting, but imperative to conduct a study to determine the incidence of the same and whether or not symptoms occur during the episode of hypoglycemia. The role of diabetes education in this juncture is very important. Explaining to patients about hypoglycemia symptoms, correction and possibility of HAAF in individuals with long standing diabetes can help reduce it’s occurrence and therefore reduce morbidity in patients who insist of relaxed glycemic goals in fer of severe hypoglycemia.
Materials and Methods
This prospective interventional study was conducted after ethical committee clearance, in AJ Institute of Medical sciences and Reseach Centre. 92 consenting individuals were recruited on a basis of a score, achieved, from Modified Clarke’s Questionnaire to reveal clinically, Hypoglycemia unawareness. Individuals with hepatic, renal or other known autonomic disturbances were excluded, as were pregnant ladies and individuals on beta blockers.
Statistics
The collected data was analyzed using mean, mode for demographic data and frequency percentage for the analysis of the clinical data. Statistical analysis was done using SPSS software version 23.0. A ‘p’ value less than 0.05 (p<0.05) is considered significant. The various measures of central tendencies and graphical representations were used to analyze the data.
Results
Over a period of one year, a total of 92 subjects with diabetes Mellitus were assessed clinically, then objectively for hypoglycemia. Of these, 72 were found to have hypoglycemia unawareness as per the modified Clarke’s questionnaire. 62 then underwent 72 hours Continuous Glucose monitoring, to objectively confirm episodes of asympotmatic hypoglycemia. A hypoglycemia index done, then showed that for every 3 symptomatic episodes of hypoglycemia, 5 episodes were asymptomatic.
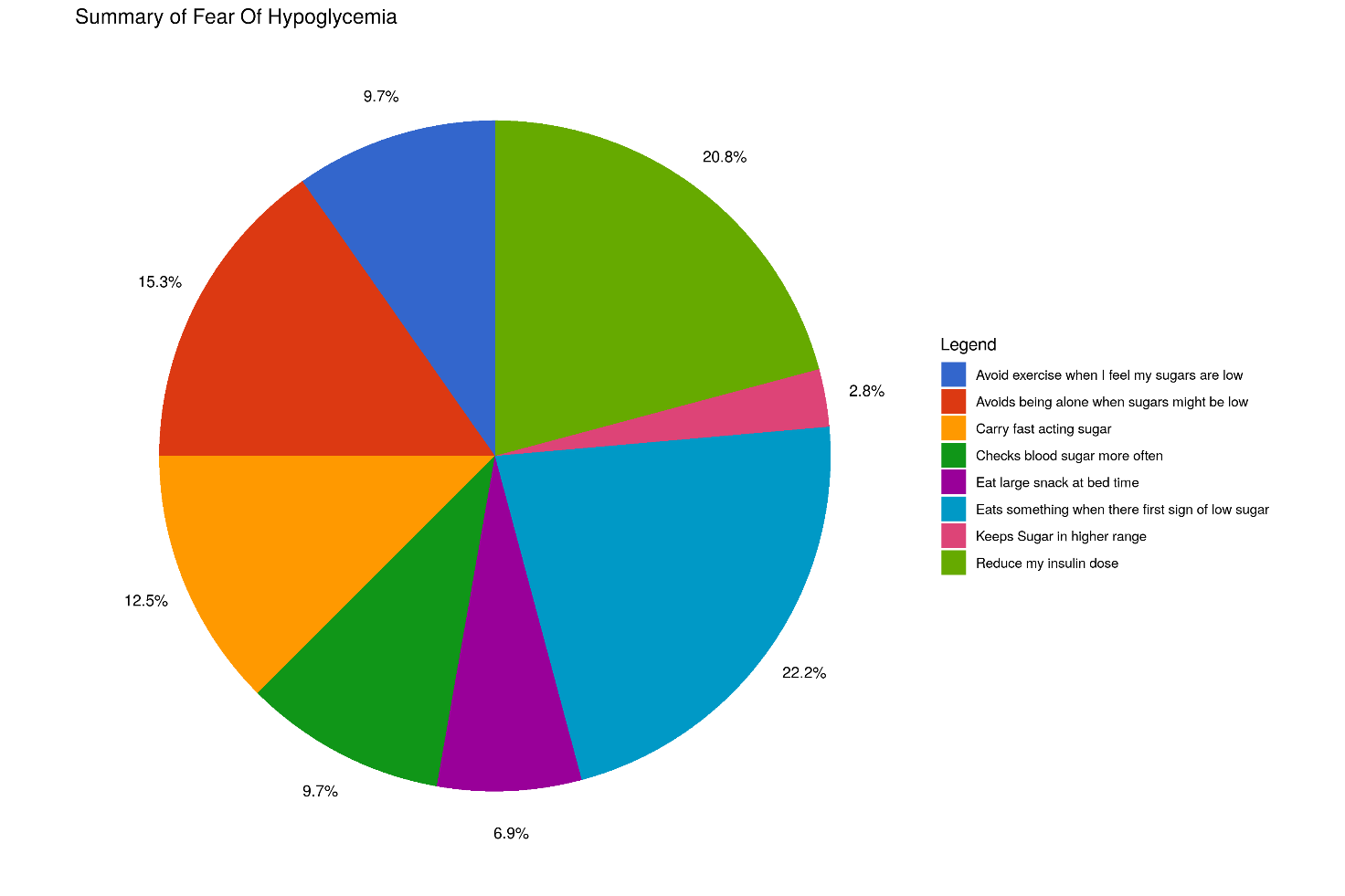
Behavioral modifications with respect to hypoglycemia
Although an individual with diabetes adapts multiple measures to prevent hypoglycemia, the most common behavior practiced by individuals with diabetes was to consume something when they feel the first sign of low sugars, followed by reducing their insulin dose. The least common strategy was to keep their sugars on the higher side.
Concern about not being able to self correct low sugars
Only two individuals were worried about not having any aid to self correct low sugars if they have symptoms. 54% were not at all worried about being able to reach for sugars when having symptoms of low sugars. This on further prompting was found to be due to lack of awareness about how to self correct - use of glucose, checking with glucometer etc.
Discussion
Hypoglycemia is an inevitable part of diabetes mellitus. Clinically the greatest risk occurs after failure of cerebral glucose supply causing progressive cognitive impairment, confusion and unconsciousness. Psychologically, it is fearful, and the burden of having to deal with hypoglycemia in public is all the more difficult to cope with.
Hypoglycemia unawareness and a previous history of episodes of severe hypoglycemia are risk factors for severe hypoglycemia. Hypoglycemia unawareness in turn is also associated with a 6 fold increased risk of severe hypoglycemia in type 1 diabetes.5
In a tertiary care center in south India, 40 individuals with type 1 diabetes clinically determined to have hypoglycemia unawareness were subjected to a CGM Study with which asymptomatic hypoglycemia was confirmed in 25% of these individuals, and 50% were nocturnal. It was concluded that a resonable individualised glycemic goal in Type 1 Diabetes Mellitus, should be the lowest A1C that preserves awareness of hypoglycemia, preferably with minimal symptomatic or even asymptomatic hypoglycemia.2
The prevalence of Hypoglycemia unawareness in a post-hoc analysis of data collected as part of the UK Hypoglycemia Group study, was found to be 22.1%.4 Frier et studied 518 subjects with diabetes with a self reported questionnaire. These subjects had retrospectively documented episodes of hypoglycemia by self monitoring of blood glucose. Hypoglycemia unawareness was present of 19.5% of this cohort.6
It is known, based on several studies that hypoglycemia can have a major impact on the quality of life. The well-being could be affected by direct effects of hypoglycemia and also indirectly from fear of recurrence.7, 8 As a result of fear, there is a tendency to modify behavior to prevent hypoglycemia, which may contribute to poor glycemic control and again attenuate their quality of life.6
There have also been several studies done to suggest that severe hypoglycemia and cognitive dysfunction go hand in hand. Asvold et al suggested that early exposure to severe hypoglycemia could have clinically relevant effects on cognition many years later. In this study the overall cognitive scores of the nine diabetic children who experienced severe hypoglycemia before age of ten were lower than the eighteen diabetic children without history of severe hypoglycemia.9
Hypoglycemia can on the other hand, place an individual at risk of unpleasant situations resulting in social embarrassment.10, 11
This study has revealed the need for further evaluation on hypoglycemia unawareness in our population in India, and individualisd goals. Diabetes education must include recognition of and apt corrective measures for hypogycemia.
Conclusion
Overall, the conclusions drawn from this study are:
Diabetes Education sessions must regularly highlight hypoglycemia recognition and management.
Quality of life (with respect to Fear of hypoglycemia) is impaired
Hypoglycemia unawareness should be included as part of assessment during every visit to the clinician
Glycemic Targets need to be individualized based on risk of hypoglycemia
Limitation
The limitations of the study were
The study was done at a tertiary care centre, hence the data may not actually represent the problems of the population at large.
The short duration and small sample size as compared to the disease burden.
We recommend that
To validate this study, a larger number of patient’s have to be studied with non-traditional risk factors.